Abstract
Research Article
Evaluation of outcomes of 8-week therapy with ledipasvir/sofosbuvir or glecaprevir/pibrentasvir in veterans with hepatitis C infection
L Anri Lemoine and Marisel Segarra-Newnham*
Published: 13 November, 2019 | Volume 3 - Issue 1 | Pages: 027-030
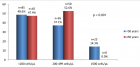
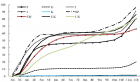
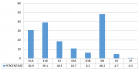
Hepatitis C Virus (HCV) infection is usually treated with direct acting antivirals (DAAs) for 12 weeks. In treatment naive patients with genotype (GT) 1 infection without cirrhosis and baseline viral load < 6 million, 8 weeks of Ledipasvir/Sofosbuvir (LDV/SOF) is an option. Eight weeks with Glecaprevir/Pibrentasvir (GLE/PIB) is an option for patients with GT 1 through 6 without cirrhosis. Our objective was to evaluate achievement of Sustained Virologic Response (SVR) after 8 weeks of LDV/SOF or GLE/PIB in our HCV-infected veterans. Patients with HCV infection that received GLE/PIB or LDV/SOF for a planned 8 weeks of therapy in the past four years were reviewed (January 2015-September 2018). Treatment outcomes were evaluated through medical record review.
Two hundred sixty-five veterans were initiated on 8 weeks of therapy with either GLE/PIB or LDV/SOF. Of these, 231 (87%) were initiated on 8 weeks of LDV/SOF and 34 (13%) were initiated on 8 weeks of GLE/PIB. The majority of patients had GT 1 (93%) infection. One hundred and ninety-five veterans who completed 8 weeks of LDV/SOF and 30 veterans on GLE/PIB had follow-up viral loads. The overall SVR was 95%. Treatment with GLE/PIB resulted in a higher SVR rate (100%) compared to LDV/SOF (95%). Elderly patients had similar SVR rates. Treatment with 8 weeks of DAA is effective in our veteran population and showed an SVR rate similar to literature reports. The SVR for patients treated with 8 weeks LDV/SOF was slightly lower than the SVR for GLE/PIB; however, the GLE/PIB population was smaller
Read Full Article HTML DOI: 10.29328/journal.acgh.1001011 Cite this Article Read Full Article PDF
References
- Centers for Disease Control and Prevention. Viral Hepatitis: Hepatitis C Information. 2019.
- Messina JP, Humphreys I, Flaxman A, Brown A, Cooke GS, et al. Global distribution and prevalence of hepatitis C virus genotypes. Hepatology. 2014; 61: 77-87. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25069599
- Abutaleb A, Kottilil S, Wilson E. Glecaprevir/pibrentasvir expands reach while reducing cost and duration of hepatitis C virus therapy. Hepatol Int. 2018; 12: 214-222. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29845496
- American Association for the Study of Liver Diseases, and Infectious Diseases Society of America. HCV guidance: recommendations for testing, managing, and treating hepatitis C. 2019
- Andres J, Lott S, Qureshi K. Eight-Week Outcomes of Ledipasvir/Sofosbuvir in Noncirrhotic Treatment-Naive Patients with Hepatitis C: Analysis of Pharmacy-Based Data. J Manag Care Spec Pharm. 2018; 24: 23-28. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29290174
- Babatin MA, AlGhamdi AS, Assiri AM, AlBiladi H, AlOthmani HS, et al. Treatment efficacy of ledipasvir/sofosbuvir for 8 weeks in non-cirrhotic chronic hepatitis C genotype 4 patients. Saudi J Gastroenterol. 2019; 25: 55-60. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30117490
- Shiha G, Esmat G, Hassany M, Soliman R, Elbasiony M, et al. Ledipasvir/sofosbuvir with or without ribavirin for 8 or 12 weeks for the treatment of HCV genotype 4 infection: Results from a randomised phase III study in Egypt. Gut. 2019; 68: 721-728. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29666174
- Kowdley KV, Gordon SC, Reddy KR, Rossaro L, Bernstein DE, et al. Ledipasvir and sofosbuvir for 8 or 12 weeks for chronic HCV without cirrhosis. N Engl J Med. 2014; 370: 1879-1888. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24720702
- Wyles D, Poordad F, Wang S, Alric L, Felizarta F, et al. (2018) Glecaprevir/pibrentasvir for hepatitis C virus genotype 3 patients with cirrhosis and/or prior treatment experience: A partially randomized phase 3 clinical trial. Hepatology. 2018; 67: 514-523. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28926120
- Rockstroh JK, Lacombe K, Viani RM, Orkin C, Wyles D, et al. Efficacy and Safety of Glecaprevir/Pibrentasvir in Patients Coinfected With Hepatitis C Virus and Human Immunodeficiency Virus Type 1: The EXPEDITION-2 Study. Clin Infect Dis. 2018; 67: 1010-1017. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29566246
- Gane E, Poordad F, Zadeikis N, Valdes J, Lin CW, et al. Safety and Pharmacokinetics of Glecaprevir/Pibrentasvir in Adults with Chronic Genotype 1-6 Hepatitis C Virus Infections and Compensated Liver Disease. Clin Infect Dis. 2019; 69: 1657-1664. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30923816
- Tavabie OD. Should we screen for cirrhosis? BMJ. 2017; 358: j3233.
- Foster GR, Asselah T, Kopecky-Bromberg S, Lei Y, et al. Safety and efficacy of glecaprevir/pibrentasvir for the treatment of chronic hepatitis C in patients aged 65 years or older. PLoS One. 2019; 14: e0208506. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30601818
Figures:

Figure 1
Similar Articles
-
A rare cause of obstructive jaundice - case reportPriya Mohan*,Sumathi Bavanandam,Sunil Kumar KS. A rare cause of obstructive jaundice - case report . . 2017 doi: 10.29328/journal.hcg.1001001; 1: 001-003
-
Anemia due to a rare anomaly - Case ReportS Nanthakumar*,Sumathi Bavanandam,Nirmala Dheivamani,Natarajan B, Krishna Mohan. Anemia due to a rare anomaly - Case Report . . 2017 doi: 10.29328/journal.hcg.1001002; 1: 004-006
-
The influence of Infliximab on the development of Experimental PancreatitisLychkova AE*,Golubev Yu Yu, Puzikov AM. The influence of Infliximab on the development of Experimental Pancreatitis . . 2017 doi: 10.29328/journal.hcg.1001003; 1: 007-011
-
Role of Accessory Right Inferior Hepatic Veins in evaluation of Liver TransplantationAwais Ahmed,Abdu Hafeez-Baig*, Mirza Akmal Sharif,Umair Ahmed,Raj Gururajan. Role of Accessory Right Inferior Hepatic Veins in evaluation of Liver Transplantation . . 2017 doi: 10.29328/journal.acgh.1001004; 1: 012-016
-
Analysis of Pyogenic Liver AbscessesEva Barreiro Alonso**. Analysis of Pyogenic Liver Abscesses . . 2018 doi: 10.29328/journal.acgh.1001005; 2: 001-004
-
Hepatic adenomatosis: A clinically challenging rare liver diseaseSunitha Ramachandra*,Lakshmi Rao, Masoud Al Kindi . Hepatic adenomatosis: A clinically challenging rare liver disease. . 2018 doi: 10.29328/journal.acgh.1001006; 2: 005-008
-
An uncommon cause of isolated ascites: Pseudomyxoma peritoneiLouly Hady*,I Nassar, K Znati,N Kabbaj. An uncommon cause of isolated ascites: Pseudomyxoma peritonei . . 2019 doi: 10.29328/journal.acgh.1001007; 3: 001-005
-
Transcatheter Arterial Embolization for the treatment of upper gastrointestinal bleedingMohammed Habib*,Majed Alshounat. Transcatheter Arterial Embolization for the treatment of upper gastrointestinal bleeding . . 2019 doi: 10.29328/journal.acgh.1001008; 3: 006-011
-
Endoscopic treatment of pancreatic diseases via Duodenal Minor Papilla: 135 cases treated by Sphincterotomy, Endoscopic Pancreatic Duct Balloon Dilation (EPDBD), and Pancreatic Stenting (EPS)Tadao Tsuji*, G Sun,A Sugiyama, Y Amano,S Mano,T Shinobi,H Tanaka,M Kubochi,K Ohishi,Y Moriya,M Ono,T Masuda, H Shinozaki,H Kaneda,H Katsura,T Mizutani, K Miura,M Katoh, K Yamafuji, K Takeshima,N Okamoto,Y Hoshino,N Tsurumi,S Hisada,J Won,T Kogiso,K Yatsuji,M Iimura, T Kakimoto,S Nyuhzuki. Endoscopic treatment of pancreatic diseases via Duodenal Minor Papilla: 135 cases treated by Sphincterotomy, Endoscopic Pancreatic Duct Balloon Dilation (EPDBD), and Pancreatic Stenting (EPS) . . 2019 doi: 10.29328/journal.acgh.1001009; 3: 012-019
-
Addition of Simvastatin to Carvedilol and Endoscopic Variceal Ligation improves rebleeding and survival in patients with Child-Pugh A and B class but not in Child Pugh C classSanjeev Kumar Jha*,Kuldeep Saharawat,Ravi Keshari,,Praveen Jha,Shubham Purkayastha, Ravish Ranjan . Addition of Simvastatin to Carvedilol and Endoscopic Variceal Ligation improves rebleeding and survival in patients with Child-Pugh A and B class but not in Child Pugh C class . . 2019 doi: 10.29328/journal.acgh.1001010; 3: 020-026
Recently Viewed
-
Success, Survival and Prognostic Factors in Implant Prosthesis: Experimental StudyEpifania Ettore*, Pietrantonio Maria, Christian Nunziata, Ausiello Pietro. Success, Survival and Prognostic Factors in Implant Prosthesis: Experimental Study. J Oral Health Craniofac Sci. 2023: doi: 10.29328/journal.johcs.1001045; 8: 024-028
-
Agriculture High-Quality Development and NutritionZhongsheng Guo*. Agriculture High-Quality Development and Nutrition. Arch Food Nutr Sci. 2024: doi: 10.29328/journal.afns.1001060; 8: 038-040
-
A Low-cost High-throughput Targeted Sequencing for the Accurate Detection of Respiratory Tract PathogenChangyan Ju, Chengbosen Zhou, Zhezhi Deng, Jingwei Gao, Weizhao Jiang, Hanbing Zeng, Haiwei Huang, Yongxiang Duan, David X Deng*. A Low-cost High-throughput Targeted Sequencing for the Accurate Detection of Respiratory Tract Pathogen. Int J Clin Virol. 2024: doi: 10.29328/journal.ijcv.1001056; 8: 001-007
-
A Comparative Study of Metoprolol and Amlodipine on Mortality, Disability and Complication in Acute StrokeJayantee Kalita*,Dhiraj Kumar,Nagendra B Gutti,Sandeep K Gupta,Anadi Mishra,Vivek Singh. A Comparative Study of Metoprolol and Amlodipine on Mortality, Disability and Complication in Acute Stroke. J Neurosci Neurol Disord. 2025: doi: 10.29328/journal.jnnd.1001108; 9: 039-045
-
Development of qualitative GC MS method for simultaneous identification of PM-CCM a modified illicit drugs preparation and its modern-day application in drug-facilitated crimesBhagat Singh*,Satish R Nailkar,Chetansen A Bhadkambekar,Suneel Prajapati,Sukhminder Kaur. Development of qualitative GC MS method for simultaneous identification of PM-CCM a modified illicit drugs preparation and its modern-day application in drug-facilitated crimes. J Forensic Sci Res. 2023: doi: 10.29328/journal.jfsr.1001043; 7: 004-010
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."