Research Article
Role of Accessory Right Inferior Hepatic Veins in evaluation of Liver Transplantation

Awais Ahmed1, Abdu Hafeez-Baig1,3*, Mirza Akmal Sharif2, Umair Ahmed2 and Raj Gururajan3
1Department of Radiology, Shifa International Hospital, Islamabad, Pakistan2Department of Internal Medicine, DHQ Hospital, Faisalabad, Pakistan
3University of Southern Queensland, Toowoomba, Queensland, Australia
*Address for Correspondence: Abdul Hafeez-Baig, Department of Radiology, Shifa International Hospital, Islamabad, Email: [email protected]
Dates: Submitted: 20 November 2017; Approved: 28 December 2017; Published: 29 December 2017
How to cite this article: Ahmed A, Baig AH, Sharif MA, Ahmed U, Gururajan R. Role of Accessory Right Inferior Hepatic Veins in evaluation of Liver Transplantation. Ann Clin Gastroenterol Hepatol. 2017; 1: 012-016. DOI: 10.29328/journal.acgh.1001004
Copyright License: © 2017 Ahmed A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Purpose: The purpose of the study is to access the prevalence of accessory right inferior hepatic veins and their relevant significance in liver transplantation.
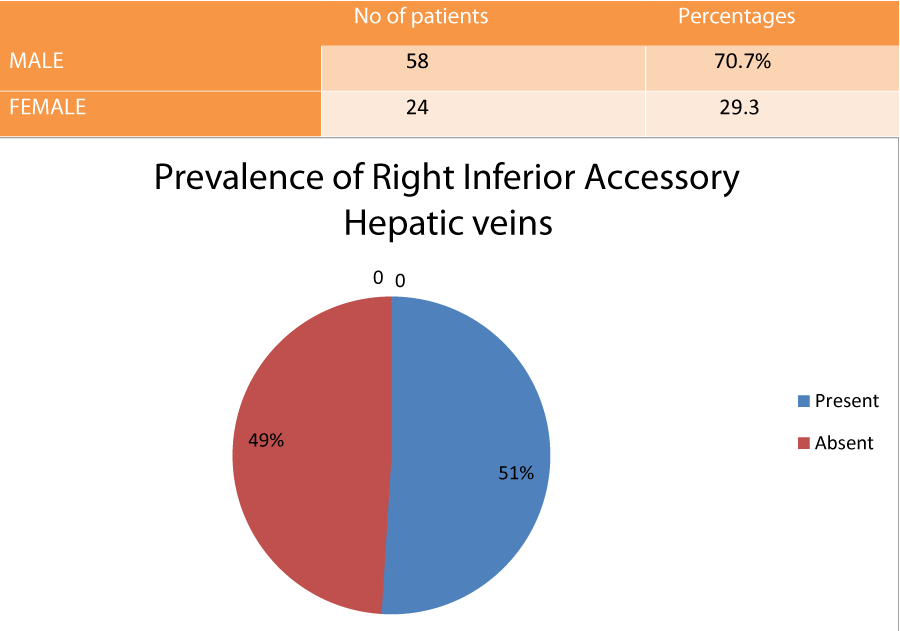
Materials and Methods: A retrospective study was done in which the CT of 82 potential liver transplant candidates between January 2012 and March 2013 were reviewed. The presence of the accessory right inferior hepatic vein was examined; the diameters of the accessory inferior hepatic veins and the distance between the point where they open into the inferior vena cava on the coronal plane and to the right hepatic vein-inferior vena cava junction was measured.
Results: Out of 82 patients, 42 (51%) had accessory right inferior hepatic veins. Right accessory inferior hepatic veins larger than 3 mm were detected in 23 (28%) patients. The distance of these veins to the right hepatic vein-inferior vena cava junction was more than 4 cm in 13 (15%) patients.
Conclusion: The precise preoperative knowledge of accessory right inferior hepatic veins is essential in living donor liver transplantation.
Introduction
The world’s first successful liver transplantation was performed by Dr Thomas Starzl in the 1960s. Since then, liver transplantation has been performed in an increasing number of patients with liver dysfunction due to chronic liver disease and acute liver failure [1]. During the past 50 years, liver transplantation has evolved from an experimental surgery of last resort to an increasingly routine procedure performed at more than 100 transplant centers in the United States and numerous other centers worldwide. According to Organ Procurement and Transplantation Network data, as of January 3, 2014, 6256 liver transplants were performed in the United States alone in 2012 [2]. Liver transplantation is one of the greatest advances of the past 3 decades for the care of patients with hepatic failure. Liver transplantation is an excellent, and sometimes lifesaving, treatment option for patients with acute and chronic end-stage organ diseases, with reported 1-year graft and patient survival rates of 80%-90% and 5-year rates of 60%-90%. Improved results of cadaveric liver transplantation have resulted in a dramatic shortage of donor liver grafts, even in countries such as Spain, where the donation rate is relatively high (33.7 per 1 million persons in 2002) [3].
To meet the needs of an increasing number of potential liver transplant recipients, alternative approaches have been developed, namely, reduced-size transplantation, split transplantation, and living donor liver transplantation (LDLT). However, LDLT may cause morbidity in an otherwise healthy donor who generously takes such an important risk for a loved one. Therefore, donor safety is a primary concern, and selection protocols are of paramount importance to preserve donor health by excluding unsuitable candidates for either medical or anatomic reasons [4]. With the development of the new multidetector computed tomographic (CT) techniques, the radiologist plays a relevant role, providing, with a minimally invasive procedure, valuable information that will be useful in choosing the most suitable candidate and in identifying anatomic variants that may alter the surgical approach. Imaging of potential donor livers is an integral step of the evaluation for potential living donor liver transplantation. Imaging can be performed using CT or MRI, and the examination encompasses calculation of liver lobe volumes and evaluation of vascular and biliary anatomy [5].
If the right inferior accessory vein is larger than 3 mm or the distance between the confluence of the main hepatic vein into inferior vena cava (IVC) and the accessory vein is more than 4 cm, the surgical approach must be altered to prevent complications such as bleeding and graft malfunction [6].
It is necessary to document if one or more than accessory right inferior hepatic veins are present. These have same importance to hepatic transplantation as large tributaries of middle hepatic vein.
Materials and Methods
After approval from Institutional Re view Board and Ethics committee, a retrospective study was done in which the CT of 82 potential liver transplant candidates between January 2012 and March 2013 were reviewed. 3-D images were obtained and image post processing was done on workstation in axial, sagittal and coronal planes. The presence of the accessory right inferior hepatic vein was examined; the diameters of the accessory inferior hepatic veins and the distance between the point where they open into the inferior vena cava on the coronal plane and to the right hepatic vein-inferior vena cava junction was measured.
Results
Out of 82 patients, 42 (51%) had accessory right inferior hepatic veins. Right accessory inferior hepatic veins larger than 3 mm were detected in 23 (54.8%) patients. The distance of these veins to the right hepatic vein-inferior vena cava junction was more than 4 cm in 13 (30.9%) patients.
Discussion
Imaging of potential donor livers is an integral step of the evaluation for potential living donor liver transplantation. Imaging can be performed using CT or MRI, and the Examination encompasses calculation of liver lobe volumes and evaluation of vascular and biliary anatomy. The latter is essential to preoperative planning; in some cases, the risks that variant anatomy present may also preclude transplantation because of the risk of intra- and postoperative complications in both the donor and recipient. Preoperative imaging of the liver enables detection of abnormalities, such as portal vein thrombosis; vascular anomalies; and biliary anatomic variants in both donors and recipients, as is illustrated by the high frequency of anatomic variants that are seen at preoperative imaging [7-9]. Three dimensional (3 D) reconstructed images are very helpful in pre-operative planning of hepatic transplantation and to avoid intraoperative and post procedure complications.
Accessory right inferior hepatic vein is the most common variation in the hepatic venous system. The accessory right inferior hepatic veins (IHVs) usually drain parts of the lateral sector of the right hemilivergraft (RHL). It is present in up to 48% of the population and drains the posterior part of the right lobe (mainly segments VI and VII) directly into the inferior vena cava (IVC). It is important to determine if an accessory inferior right hepatic vein is present: If it is, a distance of 4 cm or more in the coronal plane between the accessory vein and the right hepatic vein may make it difficult to surgically implant both veins with a single occluding clamp on the recipient inferior vena cava (IVC). Accessory hepatic veins with a caliber of 5 mm or more require separate anastomosis to inferior vena cava (IVC) to prevent hepatic congestion [9].
In transplantation surgery, a road map of the biliary and arterial vascularity of the donor and recipient is a prerequisite for the procedure. Proper venous outflow reconstruction is essential for the success of living donor liver transplantation (LDLT). It has also a decisive impact on postoperative graft dysfunction. In the classic hepatic venous anatomy, three main hepatic veins drain into the inferior vena cava (IVC). The left hepatic vein drains segments II and III, the middle hepatic vein drains segments IV, V, and VIII, and the right hepatic vein drains segments V-VII. In approximately 60% of the population, the middle and left hepatic veins join to form a common trunk, which drains separately into inferior vena cava (IVC) [10].
In a study by Radtke A et al. [11], 51% of the donors had donors had inferior hepatic veins (IHV) with detectable venous drainage territories? The results of this study were similar to what we observed in our potential liver transplant donors. In another study by Kalayci et al. [12], Mulidetecter CT scan was used to identify variations in hepatic veins of potential liver transplant donors and it was found that accessory inferior right hepatic veins was found in 55 % of the potential donors.
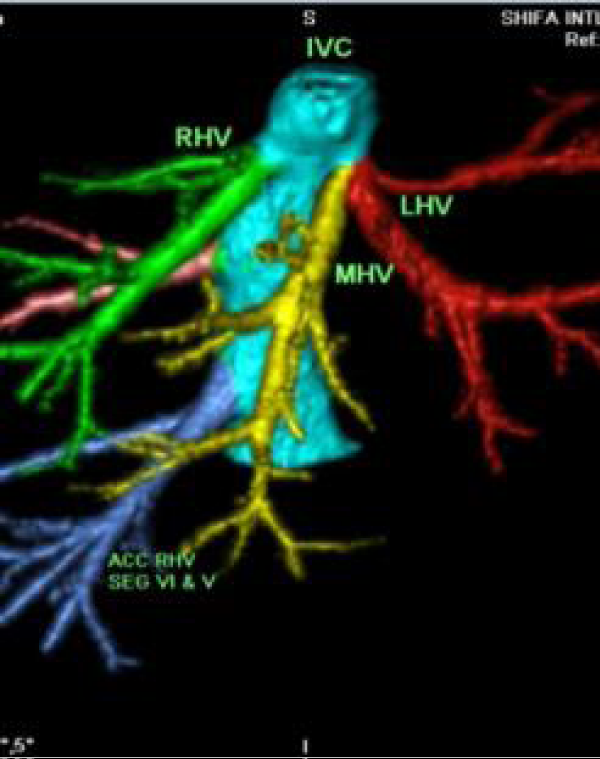
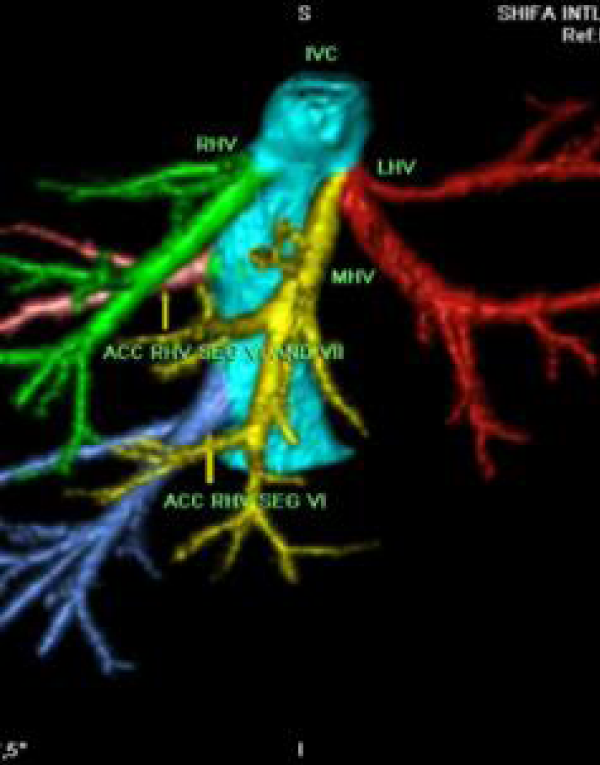
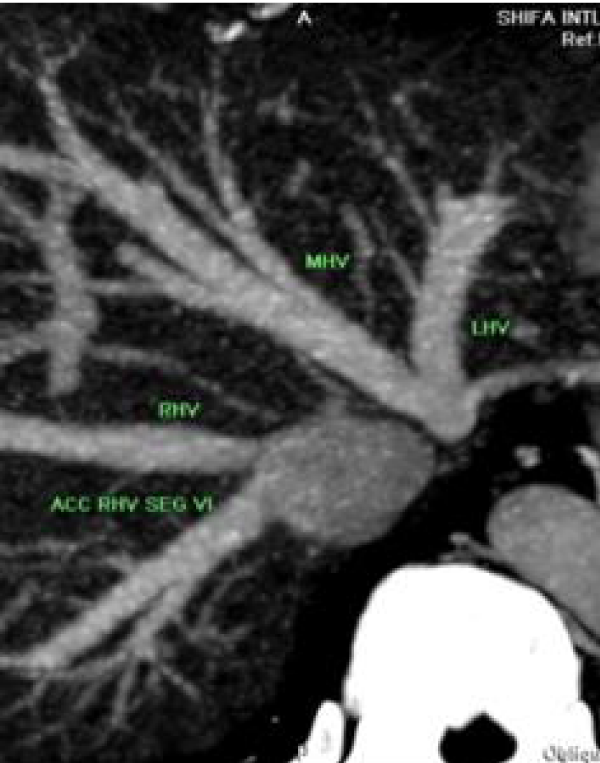
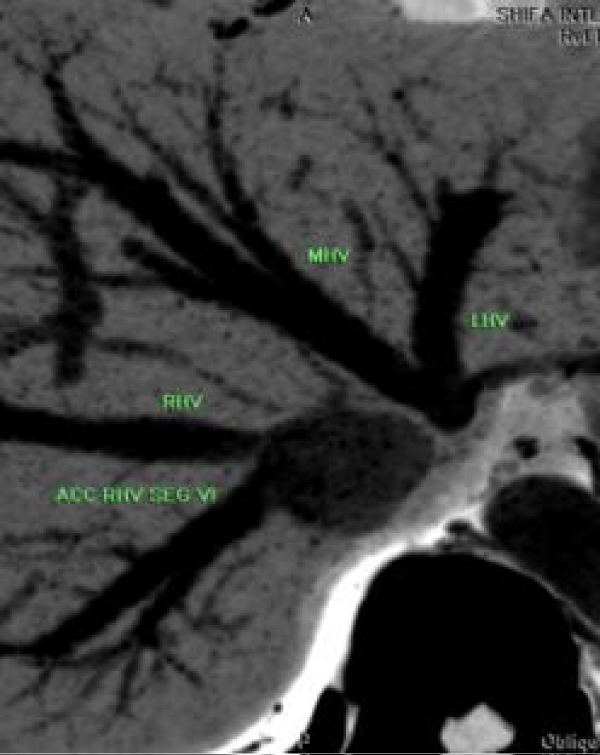
In preoperative planning, it is important to highlight not only the presence and number of these accessory veins but also their size and their distance from the main hepatic venous drainage site along the IVC. When this distance is more than 40 mm, it may be technically difficult to implant both veins into the recipient’s IVC [13]. Accessory veins are anastomosed directly to inferior vena cava (IVC) in an end-to-side fashion in liver recipient while inferior vena cava (IVC) is clamped. The inferior vena cava is clamped above and below the orifice of the right hepatic vein and the sites of anastomosis of the accessory hepatic veins [14]. Failure to recognize accessory inferior hepatic veins can lead to inadequate venous outflow. Inadequate venous out flow and congestion can result in varying degrees of graft dysfunction, including rapid progressive liver failure with graft loss [15] (Figures 1-5) (Table 1).
Figure 1: Oblique Maximum intensity projection (MIP) image showing accessory right inferior hepatic vein originating separately from inferior vena cava (IVC).
Figure 2: 26 year old man with normal liver function tests who was liver donor candidate. Oblique Maximum intensity projection (MIP) image of the patient showing two accessory right inferior hepatic veins.
Figure 3: Inverted Maximum intensity projection (MIP) image of above described patient showing two accessory right inferior hepatic veins.
Figure 4: Minimum intensity projection (MinIP) image of same patient showing two accessory right inferior hepatic veins.
Conclusion
The precise preoperative knowledge of accessory right inferior hepatic veins is essential in living donor liver transplantation. Failure to identify accessory inferior hepatic veins can lead to inadequate venous outflow, venous congestion, graft dysfunction, graft loss and liver failure.
References
- Ajay K. Singh, Arun C. Nachiappan, Hetal A. Verma, Raul N. Uppot, Michael A. Blake, et al. Postoperative Imaging in Liver Transplantation: What Radiologists Should Know. Radiographics. 2010; 30: 339-351. Ref.: https://goo.gl/iFhFZ6
- Juan C. Camacho, Courtney Coursey-Moreno, Juan C. Telleria, Diego A. Aguirre, William E. Torres, et al. Nonvascular Post-Liver Transplantation Complications: From US Screening to Crosssectional and Interventional Imaging. Radiographics. 2015; 35: 87-104. Ref.: https://goo.gl/tQ7gMK
- Ioannou GN. Development and validation of a model predicting graft survival after liver transplantation. Liver Transpl. 2006; 12: 1594-1606. Ref.: https://goo.gl/FDd1FE
- Lewis D. Hahn, Sukru H. Emre, Gary M. Israel. Radiographic features of Potential Liver Donors that Precluded Donation. American Journal of Roentgenology. 2014; 202: W343-W348.
- Ana Alonso-Torres, Jaime Fernández-Cuadrado, Inmaculada Pinilla, Manuel Parrón, Emilio de Vicente, et al. Multidetector CT in the Evaluation of Potential Living Donors for Liver Transplantation. Radiographics. 2005; 25. Ref.: https://goo.gl/5DNcbf
- Sahani D, Mehta A, Blake M, Prasad S, Harris G, et al. Preoperative Hepatic Vascular Evaluation with CT and MR Angiography: Implications for Surgery. Ridographics. 2004; 24: 1367-1380. Ref.: https://goo.gl/g45FXW
- TsangLL, ChenCL, HuangTL, T.-Y.Chen, C.-C.Wang, et al. Preoperative imaging evaluation of potential living liver donors: reasons for exclusion from donation in adult living donor liver transplantation. Transplant Proc. 2008; 40: 2460-2462. Ref.: https://goo.gl/htVi6R
- SahaniD, MehtaA, BlakeM, PrasadS, HarrisG, SainiS. Preoperative hepatic vascular evaluation with CT and MR angiography: implications for surgery. RadioGraphics.2004; 24:1367-1380. Ref.: https://goo.gl/g45FXW
- CoveyAM, BrodyLA, GetrajdmanGI, SofocleousCT, BrownKT. Incidence, patterns, and clinical relevance of variant portal vein anatomy. AJR Am J Roentgenol. 2004; 183: 1055-1064. Ref.: https://goo.gl/S3XkEH
- Onofrio A. Catalano, Anandkumar H. Singh , Raul N. Uppot, Peter F. Hahn, Cristina R. Ferrone, et al. Vascular and Biliary Variants in the Liver: Implications for Liver Surgery. Radiographics. 2008; 28: 359-378. Ref.: https://goo.gl/kdQHbJ
- Radtke A, Sotiropoulos GC, Molmenti EP, Nadalinl S, Schroeder T, et al. The influence of accessory right inferior hepatic veins on the venous drainage in right graft living donor liver transplantation. Hepatogastroenterology. 2006; 53: 479-483. Ref.: https://goo.gl/xgaufq
- Kalayci TO, Katlu R, Karasu S, Yilmaz S. Investigation of right lobe hepatic vein variations of donor using 64-detector computed tomography before living donor liver transplantation. Turk J Gastroenterol. 2014; 25: 9-14. Ref.: https://goo.gl/6bXMnf
- Erbay N, Raptopoulos V, Pomfret EA, Kamel IR, Kruskal JB. Living donor liver transplantation in adults: vascular variants important in surgical planning for donors and recipients. AJR Am J Roentgenol. 2003; 181: 109-114. Ref.: https://goo.gl/pboVge
- Amaedo M, John MH, Robert AF, Ann TO, Marc PP. Surgical Management of Anatomical Variations of the Right Lobe in Living Donor Liver Transplantation. Ann Surg. 2000; 231: 824-831. Ref.: https://goo.gl/SSj3pc
- Parrilla P, Sanchez-Bueno F, Figueras J, Jaurrieta E, Mir J, et al. Analysis of the complications of the piggyback technique in 1112 liver transplants. Transplant Proc. 1999; 67: 1214-1217. Ref.: https://goo.gl/2L3UxF