Research Article
Endoscopic treatment of pancreatic diseases via Duodenal Minor Papilla: 135 cases treated by Sphincterotomy, Endoscopic Pancreatic Duct Balloon Dilation (EPDBD), and Pancreatic Stenting (EPS)

Tadao Tsuji1*, G Sun1, A Sugiyama1, Y Amano1, S Mano1, T Shinobi1, H Tanaka1, M Kubochi1, K Ohishi1, Y Moriya1, M Ono1, T Masuda1, H Shinozaki2, H Kaneda2, H Katsura2, T Mizutani2, K Miura2, M Katoh2, K Yamafuji3, K Takeshima3, N Okamoto3, Y Hoshino4, N Tsurumi4, S Hisada4, J Won4, T Kogiso4, K Yatsuji4, M Iimura4, T Kakimoto5 and S Nyuhzuki6
1Saitama Cooperative Hospital, Gastroenterology, Japan
2Saitama City Hospital, Gastroenterology, Japan
3Saitama City Hospital, Surgery, Japan
4Tokyo Women’s Medical University, Gastroenterology, Japan
5Higashi-Toukatsu Hospital, Gastroenterology, Japan
6Higashi-Toukatsu Hospital, Gastroenterology, Japan
*Address for Correspondence: Tadao Tsuji, Saitama Cooperative Hospital, Gastroenterology, Saitama-ken Kawaguchi-Shi Kizoro, 1317, Japan, Tel: 081-48-296-4771; Email: [email protected]
Dates: Submitted: 20 June 2019; Approved: 05 July 2019; Published: 08 July 2019
How to cite this article: Tsuji T, Sun G, Sugiyama A, Amano Y, Mano S, et al. Endoscopic treatment of pancreatic diseases via Duodenal Minor Papilla: 135 cases treated by Sphincterotomy, Endoscopic Pancreatic Duct Balloon Dilation (EPDBD), and Pancreatic Stenting (EPS). Ann Clin Gastroenterol Hepatol. 2019; 3: 012-019. DOI: 10.29328/journal.acgh.1001009
Copyright License: © 2019 Tsuji T, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Minor Duodenal Papilla; Pancreatic Divisum; EPST; EPDBD-Endoscopic Pancreatic Duct Balloon Dilation; EPS; Pancreatic Stone; Pancreatic pseudocyst
Abstract
Treatments via the minor papilla is effective where the deep cannulation via the major papilla is impossible in such cases as [1] the Wirsung’s duct is inflammatory narrowed, bent or obstructed by impacted stones [2] pancreatic duct divisum (complete or incomplete) [3], maljunction of pancreatico-biliary union with stones [4], pancreatic stones in the Santorini’s duct. In [1,2] cases, the pancreatic juice flow via the major papilla decreases, while that of the minor papilla increases. Then the size of minor papilla and its orifice shows corresponding enlargement. This substitutional mechanism is an advantage when undertaking our new method. Since the pancreatic juice flow is maintained via the minor papilla in these cases, accurate and careful endoscopic skills are necessary to prevent pancreatitis due to the occlusion of the Santorini’s duct after this procedure. We have experienced 135 cases treated via minor papilla in these 27 years, so we would like to report about its safety and efficacy.
Introduction
Occasionally we experience some cases where the Wirsung’s duct is narrowed, bent and obstructed, so deep insertion of the guide wire and the catheter via the major papilla is impossible. In such cases, the minor papilla is usually enlarged and its orifice is opened. These points are the advantages to accomplish our new treatments. We have experienced 135 cases of pancreatic diseases treated via the minor papilla in these 27 years. We would like to report about its indications, methods, efficacy, safety, complications and prognoses.
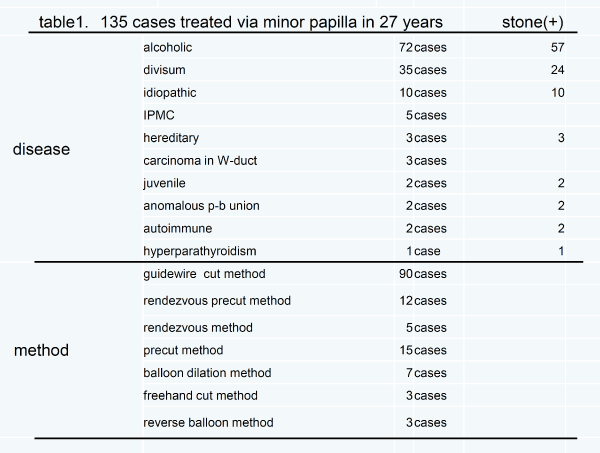
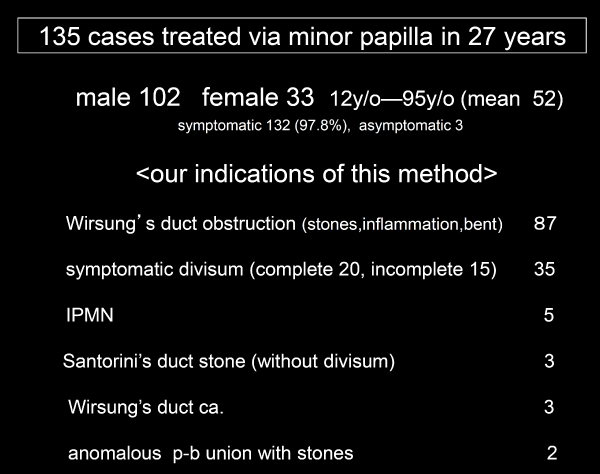
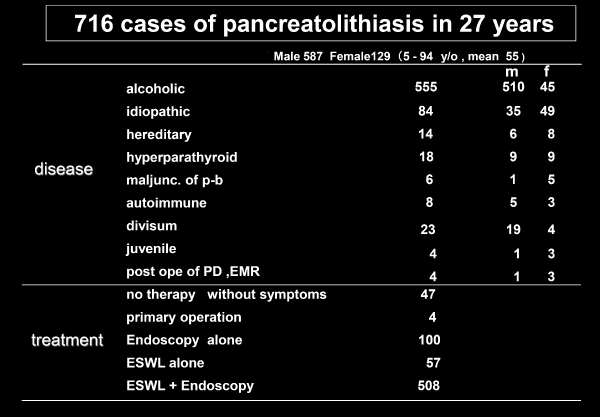
135 cases treated via minor papilla in our hospital
These 135 cases consisted of 72 alcoholic, 35 divisum, 10 idiopathic, 5 IPMC, 3 hereditary pancreatitis, 3 pancreas cancer, 2 juvenile pancreatitis, 2 maljunction of pancreato-biliary union, 2 autoimmune pancreatitis, and 1 hyperparathyroidism (Table 1) (Some patients have more than one findings). The reasons for choosing this new methods are [1] inflammatory constriction, bending, or stone impaction in the Wirsung’s duct (87 cases) [2], divisum (complete 20, incomplete 15 cases) [3], IPMC with widened opening of the minor papilla (5 cases) [4] stones located in the Santorini duct (3 cases) [5], pancreatic cancer confined to the Wirsung’s duct (3 cases) and [6] maljunction of pancreatico-biliary union with stones (2 cases) (Table 2). These 135 cases consisted of 2.6% of ERCP series in this period [1-4].
Method of treatment
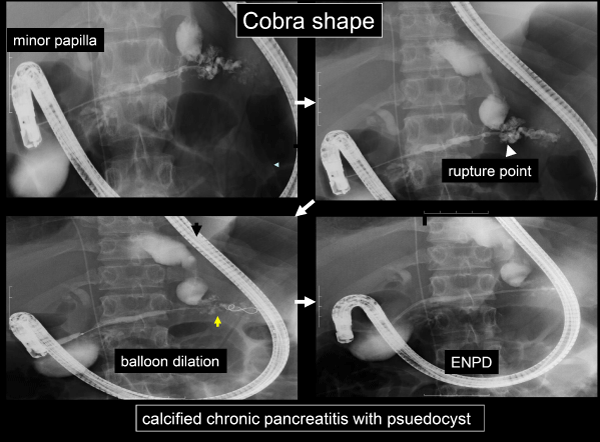
We tried our new procedures under good informed consent that if necessary the minor papilla will be cut which has the same complication rate as that of major papilla. Recently we check the status of pancreas duct by MRCP before treatment. As a treatment technique, a combination of minor papilla sphincterotomy, endoscopic pancreatic duct balloon dilation (EPDBD), and stent placement (EPS) was used. -90 cases by guidewire cut method, 15 pre-cut method, 12 rendezvous pre-cut method, 7 balloon method alone, 5 rendezvous method, 3 free hand method 3 reverse balloon method. These therapies require a significant degree of technical expertise because the minor papilla is the main route of pancreatic juice flow (Table 1) [5-8]. Minor papilla is usually located in 2-3 cm oral side and slight anterior aspect to major papilla. It is difficult to see the front face of the minor papilla when the endoscope is in a stretch position but relatively easy to view it when a intermediate position between stretch and push (we call it “cobra type position”) (Figure 1).
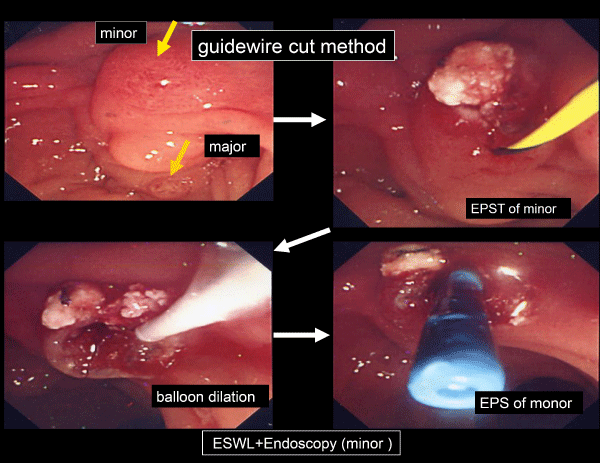
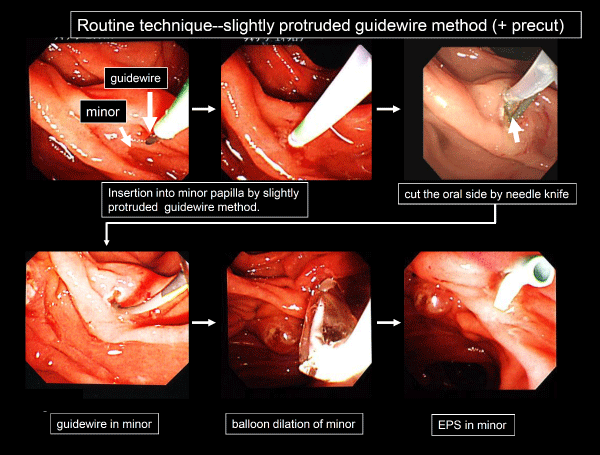
A. Guide wire cut method: 90 cases (Figure 2)
After imaging the Santorini duct, insert the catheter together with the guide wire (jagwire 0.035, 0.025 inch. Boston Scientific, radifocus guidewire 0.035inch. Terumo).
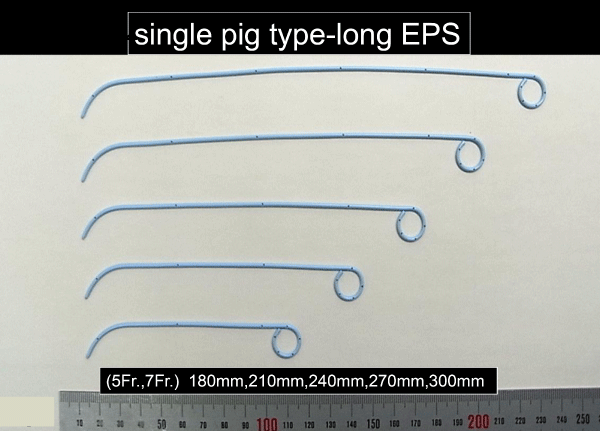
Usually we use normal type catheter (RX ERCP cannula 8.5.Fr tapered tip. 210cm Boston Scientific). If the catheter is unstable during insertion into the orifice of the Santorini’s duct, inserting with the guide wire tip protruding slightly ahead of the tip of the catheter will make the insertion easier (guide wire little-protruded method) (Figure 3). Insert the papillotome along the guide wire and slowly incise the minor papilla within the range (2-3mm) of the oral protrusion, using the same setting as for EST of the major papilla. Next, insert the guide wire deeply and the dilation balloon (Boston Scientific, Rapid dilation balloon) is advanced into the orifice of the minor and the dilation of the stricture is done. This is usually performed several times for several minutes at 4 to 6 atmospheres of pressure. We apply analgesics if necessary while checking the level of pain. Compared to the major papilla incision, the width of incision that can be made in the minor papilla is smaller, so dilation with a balloon is usually necessary. If the procedure is performed without incision, the opening is occasionally insufficient and re-insertion of the catheter may be difficult at a later date, so making both incision and balloon dilation are usually necessary. Small stones, fragmented by ESWL, are removed by basket catheter and stone-extraction balloon. EPS is then placed with Zimmon, Geenen, or more recently, our original single pig tail type (Figure 4).
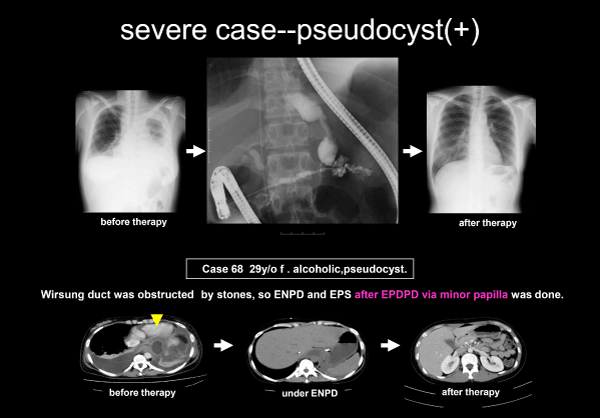
Case 1: 29 year old female: Alcoholic chronic pancreatitis, pancreatic stones, pancreatic ascites, pleural effusion, and pseudocyst-abscess. The patient was hospitalized with abdominal pain, fever, and respiratory distress. Since the Wirsung’s duct was full of stones and obstructed, the minor papilla was incised using the guide wire cut method and the body of the narrowed pancreatic duct was dilated with a balloon, then ENPD was placed. Fungus was detected in the pancreatic juice culture. After draining, the ascites and abscess rapidly disappeared and the patient was discharged (Figure 5).
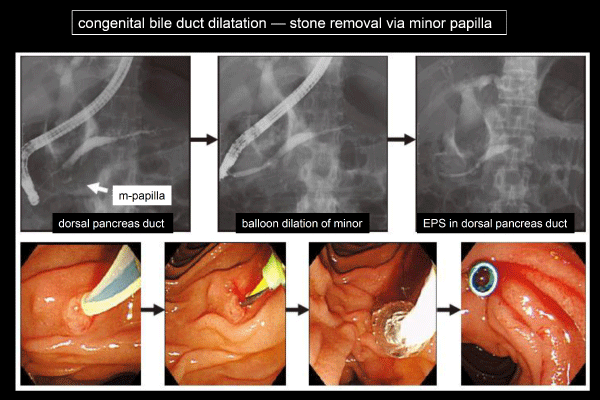
Case 2: 53 year old female: A-L1 type congenital bile duct dilatation, pancreatic stones the patient was hospitalized with abdominal pain and we tried to extract stone fragments endoscopically after ESWL. The pancreatic duct of the head is linearly narrowed due to pancreatico-biliary maljunction, deep cannulation via the major was not possible. Therefore, the minor was excised using the guidewire cut method and balloon dilation, stones were extracted and EPS was placed successfully (Figure 6).
B. Rendezvous method: 5 cases
When the Wirsung’s duct is highly angled, the guide wire sometimes passes through the minor and reverses into the duodenal cavity. In such cases, the reversed guide wire can be grasped with a snare and pulled out through the endoscope. Then a catheter can be guided into the minor after which subsequent treatment is the same as above.
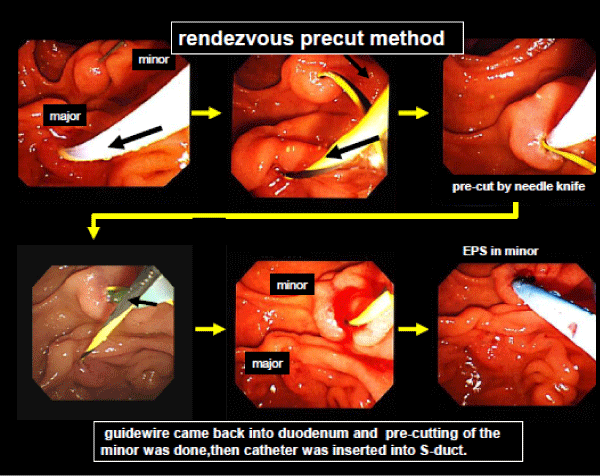
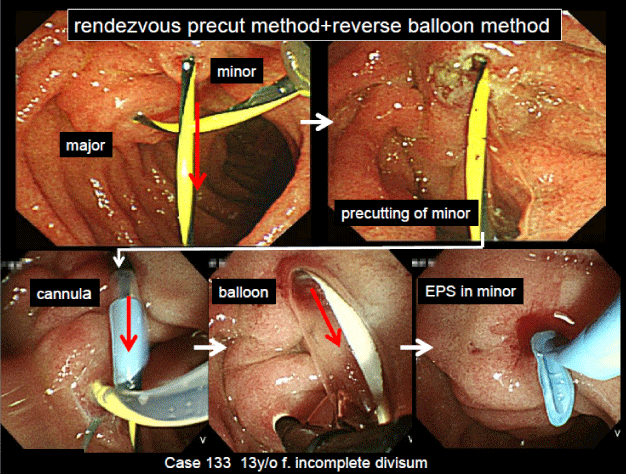
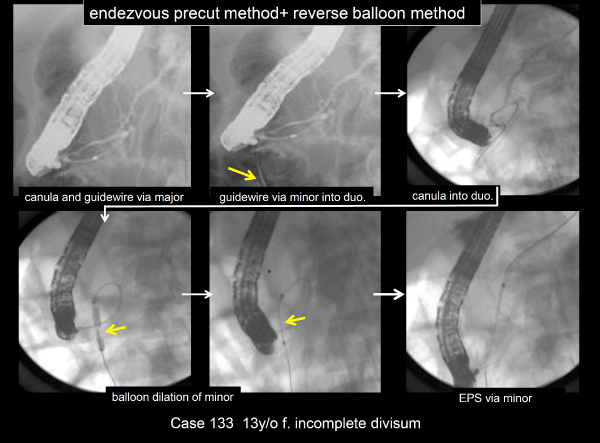
C. Rendezvous pre-cut method: 12 cases (Figure 7)
This is our original, variant procedure of the modified rendezvous method. The guidewire reversed from the minor into the duodenal cavity is the landmark to precut the minor. The minor is incised with a needle type sphyncterotome KD-200Q-0721 Olympus) and the catheter can advance into the minor.
Figure 7: Guidewire came back into duodenum and pre-cutting of the minor was done, then catheter was inserted into S-duct.
Case 3: 56-year old male: The guide wire, inserted through major papilla, came out into duodenum via minor papilla. Along this guide wire, minor papilla was cut by needle type papillotome, and the catheter was inserted into the minor papilla, then EPS was placed.
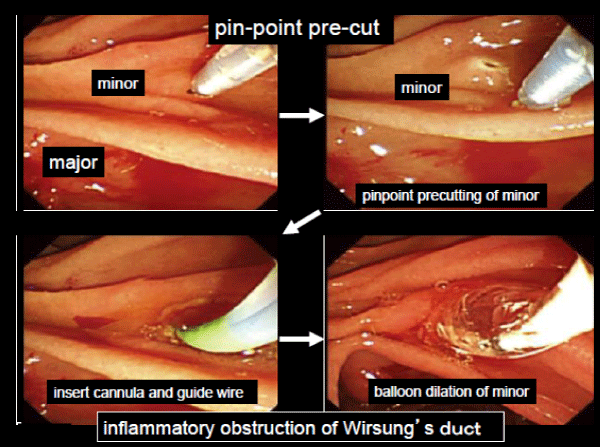
D. Precut method: 15 cases
Another method that can be used when the minor is very small, a pinpoint precut of the minor is performed and then by the guide wire-cut method, EPS is placed.
Case 4: 63-year old male: Idiopathic chronic pancreatitis, pacreatic stones. Deep cannulation was impossible due to marked narrowing of the Wirsung’s duct. Minor was too small to insert the guidewire, so pinpoint pre-cut of minor was performed, then deep cannulation was done and stones were removed after balloon dilation (Figure 8).
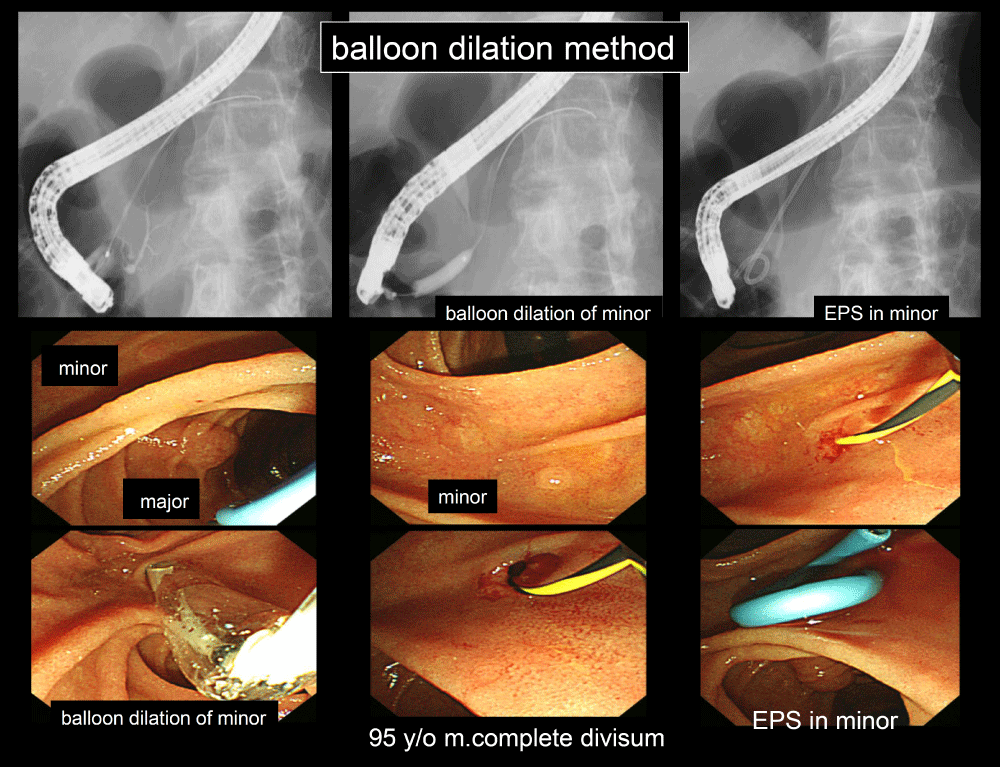
E. Balloon dilation alone method: 7 cases (Figure 9)
When the guide wire was inserted into minor papilla easily, its balloon dilation was done without cutting and EPS was placed.
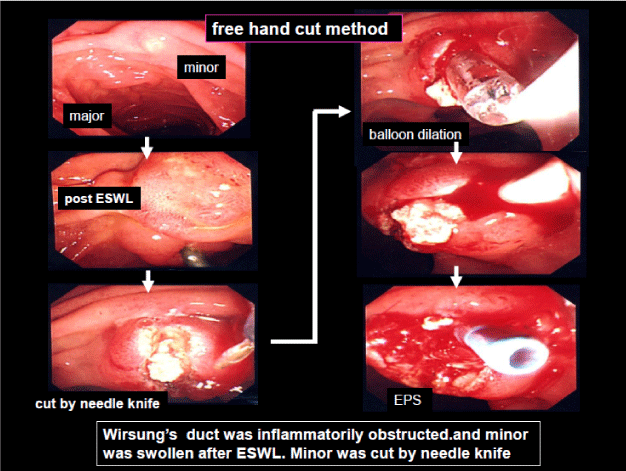
F. Free hand cut method: 3 cases (Figure 10)
In any of the above methods, when the catheter cannot be inserted into the minor papilla, an incision can be carefully made in the medial direction of the minor papilla with a pre-cut needle after which the guide wire-cut method is used. In figure 10, a remarkably swollen minor papilla is being carefully cut from down to up and stones removed.
Figure 10: Free hand cut method: Wirsung’s duct was inflammatorily obstructed and minor was swollen after ESWL. Minor was cut by needle knife.
G. Reverse balloon method: 3 cases
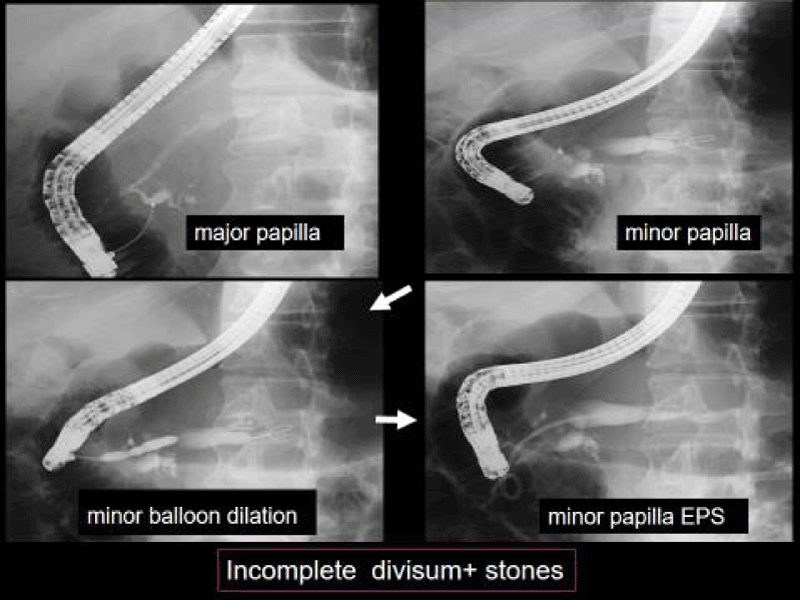
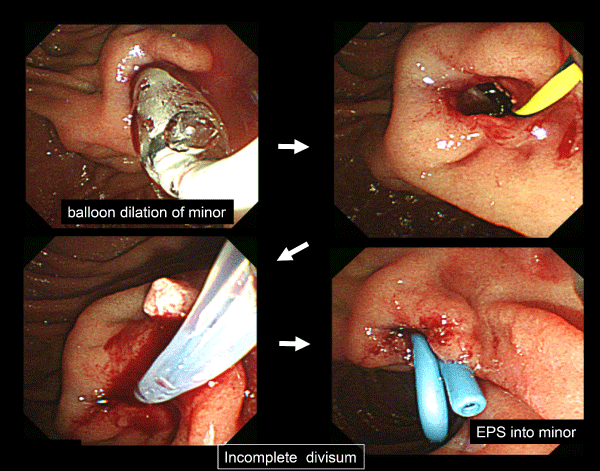
In incomplete divisum cases, the guide wire, inserted into major papilla, come out via Wirsung’s duct, connecting branch, Santorini’s duct and minor papilla into duodenum. Minor papilla was dilated by 4mm dilation balloon, then EPS could be placed into dorsal duct.
Case 5: 13-year old female: Incomplete divisum. She entered into our hospital complaining of reccurent epigastralgia. The orifice of the minor papilla was dilated by this method, then EPS was placed deeply via minor papilla (Figures 11,12).
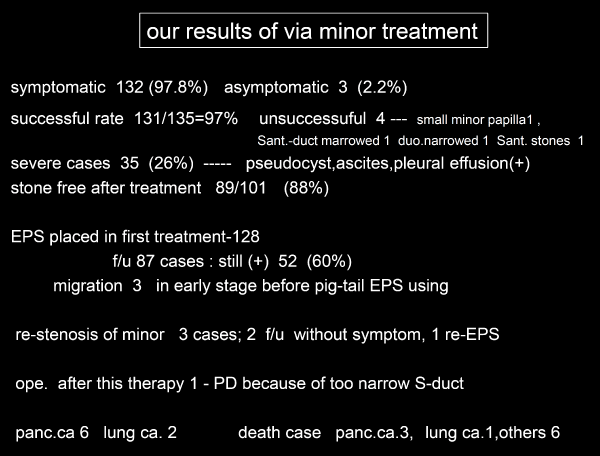
Results of the treatment via minor papilla
In these 27 years, we have treated 135 cases via minor papilla endoscopically -102 male and 33 female. Age 12 y/o (juvenile pancreatitis) to 95 y/o (complete divisum): mean age 52 y/o. Table 2 shows our indications, and Table 1 shows our treatment methods. Balloon dilation, rendezvous pre-cut,reverse balloon, and freehand method are our original procedures. We were successful in stone removal and stenting in 131 cases (131/135=97%). Symptomatic cases before therapy are 132(133/135=97.8%) with pain free in 130 cases after therapy. 4 unsuccessful cases consisted of [1] small minor papilla, [2] duodenal narrowing, [3] very narrow Santorini’s duct and [4] stones in Santorini’s duct.
Pancreatic stone treatment: Pancreatic stone cases treated by this method consisted of 97 male and 4 female. Stone free is 89 cases (88%). 665 pancreatic stone were treated medically (endoscopy and/or ESWL) in our hospital these 27 years with stone-free rate 75.2%, pain-free rate 97.1%, and a stone recurrence rate 5.0%. The pain-free rate is relatively high, but the stone-free rete is somewhat low (Table 3) [9,10]. So, as a method to raise this stone-free rate, we started our new treatment via the minor. Its stone-free rate was 98%, and the pain- free rate 100% in our series. Our new methods contributed to raise the stone removal rate.
Divisum treatment: We experienced 32 divisum cases consisited of complete type 22 (stone (+) 22) and incomplete type 10 (stone (+) 8). We treated 24 cases endoscopically via minor papilla, and achieved complete stone free and pain free in 22 cases (Figures 13,14).
Severe pancreatitis treatment: 35 severe cases complicated with pseudocyst, abscess, pancreatic pleural effusion and ascites, which were unable to be treated via major papilla were managed successfuly via minor papilla. This method contributed greatly in treating severe pancreatitis treatment (Figure 5).
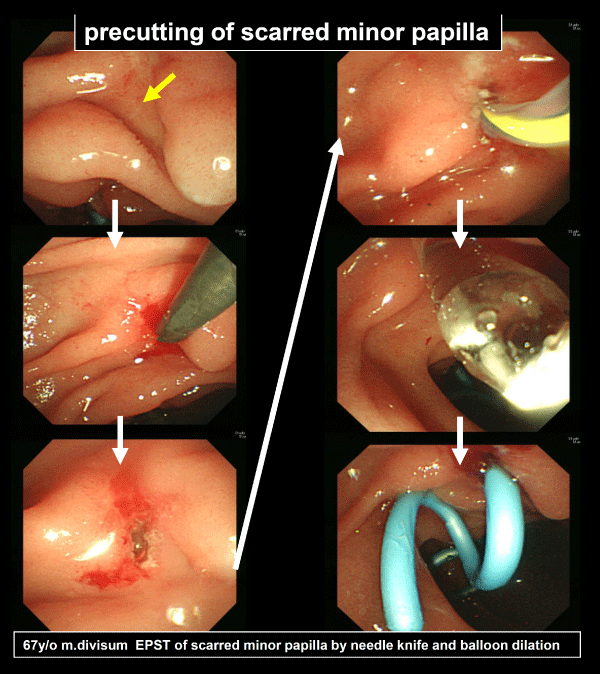
Course after this treatment: EPS was placed in 128 cases at the first treatment. 4 months and 14 months later, EPS was removed and if stenotic portion of the duct still existed, EPS was re-placed. As with the placement of EPS in the major papilla, long-term placement in Santorini’s duct has a high risk of obstructive dorsal pancreatitis. When abdominal pain occurred, EPS was withdrawn immediately and EPS was re-placed. 52 cases out of 87 cases (52/87=60%), were followed up, for 5 months to 27 years, had EPS-replacement many times and still now EPS(+). We have experienced 3 cases of EPS migration in early period, but after using pig tail type EPS, the migration of EPS doesn’t occur (Figure 4). After treatment via minor papilla, 4 cases had operations-2 pseudocyst case by pancreatic tail resection, 1 which had marked narrowing in the Santorini’s duct by pancreato-duodenal resection. 6 pancreatic and 2 lung cancer occurred and death cases were 3 pancreatic, 1 lung cancer and 6 others (Table 4). Stenosis of the minor papilla after EPS removal occurred in 3 cases in 1 case EPS was re-placed by precutting and balloon dilation method (Figure 15), 2 cases had no therapy without symptoms.
Discussion
Minor papilla is generally located approximately 2-3cm cephalad and slightly anterior to the major papilla in anterior wall of duodenum. Its size is usually very small and orifice is obscured, so the endoscopic treatment via the minor papilla is usually difficult [11,12]. There were few reports about the treatment via the minor papilla, and also few reports about the standard techniques and its indications.
In divisum cases, which is the most common anatomical anomaly, the minor papilla is swollen and bulging, so it is good indication of this treatment. Endoscopic sphincterotomy of the minor papilla in divisum cases was first reported by Cotton in 1978. Since then, many useful results have been reported. Its aim is the diagnosis of divisum and decompression of the dorsal duct by EPS insertion into the Santorini’s duct [13-23]. In 1999, Renzulli first reported about stone removal via minor papilla in divisum cases [24].
About the non- divisum cases, there are also few studies concerning via-minor- papilla interventions in the literature. In 1986, Kinukawa reported 3 cases of chronic pancreatitis treated via minor papilla by needle type papillotome. Their indication was 1 divisum, 2 severe chronic pancreatitis, 3 relapsing alcoholic chronic pancreatitis [25]. After these reports, the usefulness of the via-minor-papilla treatment in such cases as swollen and bulging minor papilla due to Wirsung’s duct obstruction, or Wirsung’s duct shows much bent shape (loop or Z type) without divisum are reported [26-28]. Ghattas, Maguchi and Sherman reported about the usefulness of the rendezvous technique [29-31]. Song reported the usefulness of the endoscopic treatment via minor papilla in 10 cases without divisum (distortion 5, stone impaction 5 with stricture of the main pancreatic duct). Their preferred choice was rendezvous method [32]. Wilcox reported that after insertion of guidewire into Santorini’s duct via minor papilla,they cut the orifice by needle type papillotome [33]. Lehman reported that after EPS placement, they cut minor papilla by needle type papillotome [18]. Kikuyama reported 12 cases treated via minor papilla (3 guide wire method, 8 cutting by needle knife method, 1 rendezvous method) [34].
In our hospital, a combination of guide wire cut method, rendezvous method, rendezvous pre-cut method, pre-cut method, balloon dilation method, free hand method, reverse balloon method were performed in 35 cases of divisum and 100 cases of other diseases. Balloon dilation method, rendezvous pre-cut method, free hand method, reverse balloon method are our original procedures. These therapies require a significant degree of technical expertise.
There are several reports about the safety and complication of this procedure. Kinukawa says that because the duodenal wall and pancreatic parenchyma are in contact at a certain width around which there is little pancreatic tissue of this procedure. Compared to a major papilla incision, there is little bleeding or postoperative inflammation when incising the minor papilla in our experience. Kinukawa says that because around the minor papilla, the duodenal wall and pancreatic parenchyma are in contact at a certain width around which there is little pancreatic tissue and no contamination with bile at the procedures, EPST of minor is safer than that of major papilla [25]. On the other hand, it is also said that pancreatic parenchyma exists in duodenal wall around the minor papilla, so EPST of minor should be performed carefully. Some authors report that the minor papilla has no arterial branch, so much bleeding after minor papilla EPST is rare [34]. Early complications of this procedure were mainly pancreatitis. About the occurrence of pancreatitis, Lehman reported 1.5% with 1 death by pancreatic abscess in cannulation failure [18], Coleman 35.2% [20], Sherman 18.8% [31], Kozarek 10.3% [35] and Cohen 13% [22,23]. Watkins reported that pancreatitis rate is 13.2%, and bleeding 1%, perforation 0.2% [36]. Their complication rate was relatively high in the literature. Compared to a major papilla incision, there is little bleeding or postoperative inflammation when incising the minor papilla in our experience.
Inui reported the usefulness of the via-minor-papilla treatment in divisum and pancreatic stone where the Wirsung’s duct is obstructed. And they recommended that these treatments should be done in selected institutions with appropriate expertise [37].
In this article, we clarified the indication of this treatment and standard techniques. Our 135 cases, the largest number in the literature, were treated by these 7 methods above. By combinations of these standard techniques, our success rate was high- 97% (131/135) compared to other reports. We experienced only 1 case of prolonged pancreatitis after ERP of which Wirsung’s duct was Z type. In other cases, no severe pancreatitis occurred. When these procedures are achieved completely, the pancreatitis after these procedures are rare, so the treatment via minor papilla is safe and very useful.
Conclusion
Endoscopic treatments of pancreatic diseases via the minor duodenal papilla are safe and very useful in [1] inflammatory constriction, bending, or stone impaction in the Wirsung’s duct [2], divisum (complete, incomplete) [3], IPMC with widened opening of the minor papilla [4], stones located in the Santorini’s duct [5], pancreatic cancer confined to the Wirsung’s duct and [6] maljunction of pancreatico-biliary union with stones. This endoscopic skill is important as therapeutic techniques in the pancreatic diseases.
References
- Tsuji T. et al. Treatment of Pancreatic diseases via duodenal minor papilla. Endoscopic treatment of bile duct and pancreas. Medical View. 2007; 158-165.
- Tsuji T. et al. Endoscopic approach-endoscopic treatment of pancreatic diseases via duodenal minor papilla Hepato-Biliary-Pancreaic Imaging. 2009; 11: 205-213.
- Tsuji T. et al. The status and the prognosis of 225 cases of pancreatic stones in our hospital. Pancreas. 2009; 24: 62-73.
- Tsuji T. et al. Treatment of Pancreatic diseases via duodenal minor papilla. Tan to Sui. 2009; 30: 1187-1194.
- Tsuji T. et al. Endoscopic treatment of pancreatic diseases via duodenal minor papilla. Tan to Sui. 2012; 33: 995-1003.
- Tsuji T. et al. Treatment of Pancreatic diseases via duodenal minor papilla. Tan to Sui. 2012; 30: 1187-1194.
- Tsuji T. et al. Endoscopic treatment of pancreatic diseases via duodenal minor papilla. Tan to Sui. 2014; 35: 249-256.
- Tsuji T. et al. 628 cases of pancreatic diseases treated by EPDBD (Endoscopic Pancreatic Duct Balloon Dilation)–its usefulness and safety. Liver and Pancreatic Sciences. 2017; 2: 1-9.
- Inui K, Tazuma S, Yamaguchi T, Ohara H, Tsuji T, et al. Treatment ofPancreatic Stones with Extracorporeal Shock Wave Lithotripsy Results of a Multicenter Survey. Pancreas. 2005; 30: 26-30. PubMed: https://tinyurl.com/yxqmeezr
- Suzuki Y, Sugiyama M, Inui K, Igarashi Y, Ohara H, et al. Management for Pancreatolithiasis A Japanese Multicenter Study. Pancreas. 2013; 42: 584-588. PubMed: https://tinyurl.com/y4ttygzo
- Kamisawa TY, Egawa. Size, location and patency of the minor duodenal papilla as determined by dye-injection endoscopic retrograde pancreatography. Dig Endosc. 2001; 13: 82-85.
- Kamisawa T. Clinical Significance of the minor duodenal papilla and accessory pancreatic duct. Journal of Gastroenterology. 2004; 39: 605-615. PubMed: https://tinyurl.com/yxq2wh75
- Cotton PB. Duodenoscopic papillotomy at the minor papilla for reccurent dorsal pancreatitis. Endoscop Digest. 1978; 3: 27-28.
- Cotton PB. Congenital anomaly of pancreas divisum as cause of obstructive pain and pancreatitis. Gut. 1980; 21: 105-114. PubMed: https://tinyurl.com/yxvts63o
- Russel RCG, Wong NW, Cotton PB. Accessory sphincterotomy endoscopic and surgical in patient with pancreas divisum. Br J Surg. 1984: 71: 954-957. PubMed: https://tinyurl.com/y5x28n8b
- Soehendra N, Kempeneers I, Nam VC, Grimm H. Endoscopic dilation and papillotomy of the accessory papilla and internal drainage in pancreas divisum. Endoscopy. 1986; 18: 129-132. PubMed: https://tinyurl.com/y67mmqt9
- Lans JI, Geenen JE, Johanson JF, Hogan WJ. Endoscopic therapy in patient with pancreas divisum and acute pancreatitis; a prospective, randomized, controlled clinical trial. Gastrointest Endosc. 1992; 38: 430-434. PubMed: https://tinyurl.com/y4nckq7t
- Lehman GA, Sherman S, Nisi R, Hawes RH. Pancreas divisum;results of minor papilla sphincterotomy. Gastrointest Endosc. 1993; 39: 1-8. PubMed: https://tinyurl.com/y42xyk7n
- Heyries L. Long term results of endoscopic management of pancreas divisum with reccurent acute pancreatitis. Gastrointest Endosc. 2002; 55: 376-381.
- Coleman SD. Endoscopic Treatment in Pancreas Divisum. The American Journal of Gastroenterology. 1994; 89: 8.
- Fukumori D, Ogata K, Ryu S, Maeshiro K, Ikeda S. An Endoscopic Sphincterotomy of the Minor Papilla in the management of Symptomatic Pancreas Divisum. Hepato-Gastoenterology. 2007; 54: 561-563. PubMed: https://tinyurl.com/y2pmy39r
- Cohen SA, Rutkovsky FD, Siegel JH, Kasmin FE. Endoscopic stenting and sphincterotomy of the minor papilla in symptomatic pancreas divisum: Results and complications. Diagn Ther Endosc. 1995; 1: 131-139. PubMed: https://tinyurl.com/yy95vxfs
- Cohen SA. A new technique of minor papilla sphincterotomy in pancreas divisum. Precut needle-knife sphincterotomy of the minor papilla in pancreas divisum. Gastrointest Endosc. 1997; 45: 155.
- Renzulli P, Müller C, Uhl W, Scheurer U, Büchler MW. Impacted papilla minor stone in pancreas divisum causing severe acute pancreatitis: A case for early ERCP in acute pancreatitis of unknown origin. Digestion. 1999; 60: 281-283. PubMed: https://tinyurl.com/y5t6qvuq
- Kinukawa K. A clinical Study of the Minor Duodenal Papilla - A Trial of the Endoscopic Papillotomy of the Minor Duodenal Papilla. Gastroenterological Endoscopy. 1986; 28.
- Arisaka Y. Endoscopic Retrograde Pancreatography via Duodenal Accessory Papilla. Tan to Sui. 2008; 29: 991-998.
- Gonoi W, Akai H, Hagiwara K, Akahane M, Hayashi N, et al. Meandering Main Pancreatic Duct as a Relevant Factor to the Onset of Idiopathic Reccurent Acute Pancreatitis. 2012; l7: e37652. PubMed: https://tinyurl.com/yygghvbt
- Koshida S. Cannulation of the Minor Papilla. Tan to Sui. 36: 925-9282015; 36: 925928.
- Ghattas G, Deviere J, Blancas JM, Baize M, Cremer M. Pancreatic rendezvous. Gastrointest Endosc. 1992; 38: 590-594. PubMed: https://tinyurl.com/y249m7xd
- Maguchi H. Approach Techniques for Pancreatic Duct in Diffi cult Cases- Rendezvous Technique and Dilation Technique of the Pancreatic Duct Stricture using a Stent Retriever. Tan to Sui. 2009; 30: 1195-1198.
- Sherman S, Lehman GA. Endoscopic Pancreatic sphincterotomy; t echniques and complications. Gastrointest Endosc Clin N Am. 1998; 8: 115-1124. PubMed: https://tinyurl.com/y26o4e
- Song MH, Kim MH, Lee SK, Lee SS, Han J, et al. Endoscopic minor papilla interventions in patients without pancreas divisum. Gastrointestinal endoscopy. 2004; 59: 901-905. PubMed: https://tinyurl.com/y47njsau
- Wilcox CM, Mönkemüller KF. Wire assited minor papilla –precut papillotomy. Gastrointestinal Endoscopy. 2001; 54; 83-86. PubMed: https://tinyurl.com/y347b65l
- Kikuyama M. Pancreatic Duct Stenting Via the duodenal Minor Papilla. Tan to Sui. 2008; 29: 1009-1015.
- Kozarek RA. Endoscopic approach to pancreas divisum. Dig Dis Sci. 1995; 40: 1975-1981.
- Watkins JL, Lehman GA. Minor papilla sphincterotomy Chapter 15) ERCP 143-151.Saunders Elsevir Philadelphia 2008.
- Inui K. Endoscopic Approach via the Minor Duodenal papilla. Digestive Surgery. 2010; 27: 153-156.