More Information
Submitted: March 17, 2021 | Approved: March 23, 2021 | Published: March 24, 2021
How to cite this article: Ghannouchi M, Chaka A, Hammouda SB, Khalifa MB, Chaouech A, et al. Giant hepatic cystadenoma mimicking a hydatid cyst: A challenging preoperative diagnosis. Ann Clin Gastroenterol Hepatol. 2021; 5: 016-017.
DOI: 10.29328/journal.acgh.1001027
Copyright License: © 2021 Ghannouchi M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Mucinous cystadenoma; Liver; Hepatic hydatid cyst type III; Degeneration; Radical treatment
Giant hepatic cystadenoma mimicking a hydatid cyst: A challenging preoperative diagnosis
Mosaab Ghannouchi1, Amina Chaka1*, Seifeddine Ben Hammouda2, Mohamed Ben Khalifa1, Asma Chaouech1, Karim Nacef1, Kamel Hleli1 and Moez Boudokhane1
1Department of Digestive Surgery, Tahar Sfar University Hospital of Mahdia 5100 & Faculty of Medecine, University of Monastir, 5000, Tunisia
2Department of Pathology, Fattouma Bourguiba University Hospital of Monastir, 5000, & Faculty of Medecine, University of Monastir, 5000, Tunisia
*Address for Correspondence: Amina Chaka, M.D, Department of Digestive Surgery, Tahar Sfar University Hospital of Mahdia 5100, Faculty of Medecine, University of Monastir, 5000, Tunisia, Tel: +216 99733261; Email: [email protected]
Biliary cystadenoma is a rare cystic tumor of the liver. It has a high recurrence rate and malignant transformation risk in middle-aged women. Pre-operative diagnosis is difficult because of the lack of clinical, biological and radiological specificity. The confirmation of the diagnosis is made by the histopathological examination. Complete surgical resection is preferred because of the high risk of malignant transformation and recurrence.
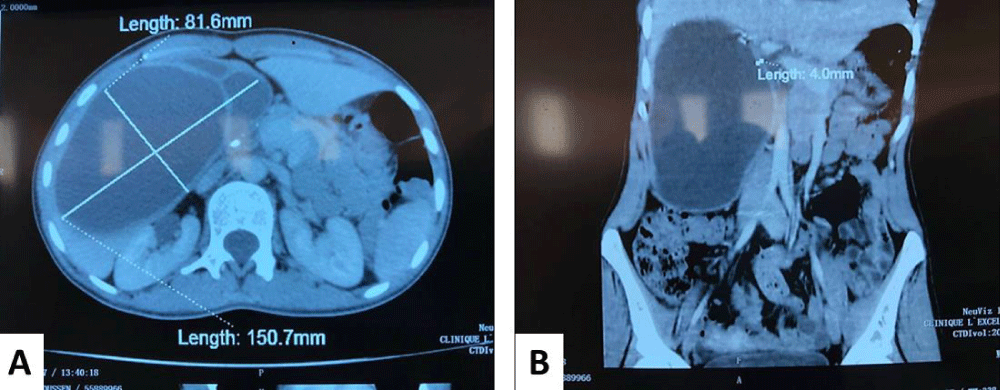
We report the case of a 66 year-old woman with no medical history, who was admitted for chronic right hypochondrium pain evolving for 3 months. Physical examination, showed an enlarged liver with no tenderness or inflammatory signs. Liver function and full blood count, were within normal limits. The hydatic serology was negative and both carcino-embryonic antigen (CEA) and α-fetoprotein tests showed normal levels. Abdominal ultrasound showed a multilocular cystic lesion of segment IV, V, VI, with an extra hepatic extension. A CT scan revealed large 15.1 x 8.7 cm cystic mass ,intra hepatic septa in segment IV, V, VI, and a 4 mm-tick wall spontaneously hyper-dense (Figure 1).
Figure 1: A, B: Abdominal CT showing a giant hepatic cyst with intrahepatic septa.
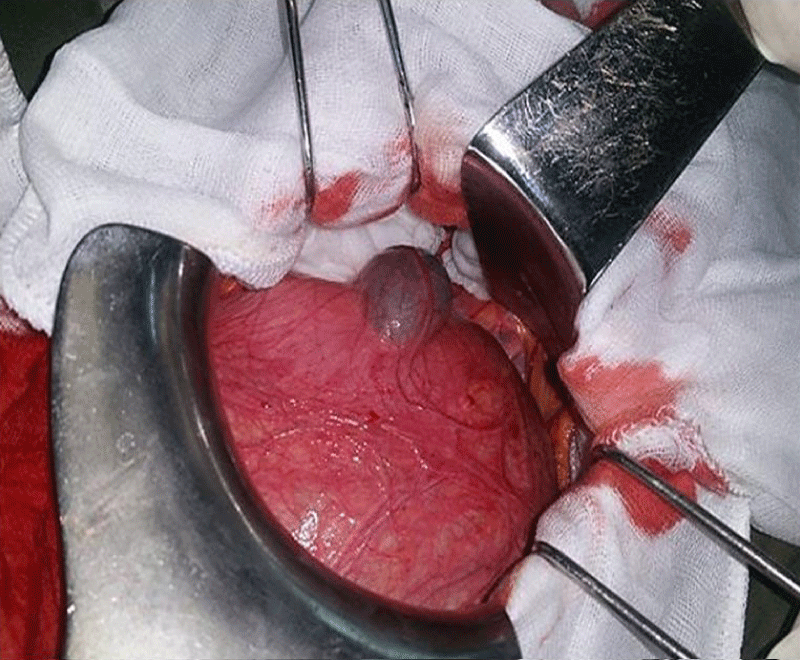
The patient underwent a laparotomy that revealed a large cyst attached to the segment V and IV (Figure 2). We performed a cholecystectomy followed by fully resection cyst.
Figure 2: Exophytic portion of the cyst attached to the segment IV and V with a hematoma contacts with the cyst.
Histopathological examination showed multiloculated cysts lined by flattened biliary type and mucinous epithelial cells with no dysplasia overlying ovarian type stroma.
Based on the above features, the diagnosis of biliary cystadenoma was given.
Biliary cystadenoma is a rare benign cystic tumor, characterized by a high risk of recurrence and malignant transformation [1]. It affects middle-aged women (40-50 years-old) [2], pediatric cases were also reported [3]. It frequently develops from the intra hepatic bile ducts, rarely from the extra hepatic bile ducts or gallbladder [4].
Clinical symptoms are not specific. An abdominal mass is frequently found. Jaundice is rarely observed and mostly reveals an intra-hepatic biliary obstruction by mucosal plugs [5]. High levels of CA19-9 or carcino-embryonic antigen (CEA) are not specific [6]. In ultrasound, the lesion appears usually as a single large mass, typically as a multilocular cyst [4].
CT scan findings show low density, lobulated, multilocular thick wall and rarely coarse calcification [7].
In MRI findings, the cyst can have a hypo intense fluid in T1 and hyper intense in T2, CT and MRI can also seek for enhancement of the capsule, septa or the presence of nodes, liver and bile ducts invasion, or carcinomatous transformation marked [4,8].
The confirmation of the diagnosis is made by the histopathological examination consisting in multiloculated cysts lined by cuboidal, columnar or flattened biliary type or mucinous epithelial cells overlying ovarian type stroma. Ovarian type stroma has densely packed, oval to spindle-shaped cells that may be focally luteinized. The cyst should be sampled extensively to rule out high grade dysplasia (complex tubulopapillary, nuclear pleomorphism, frequent mitotic figures...) and invasive carcinoma (usually ductal adenocarcinoma) [9].
The most differential diagnoses are infected or hemo-rrhagic biliary cysts, hydatid cysts, abscesses and metastases.
Radical surgery is preferred because of their potential malignancy [10]. According to the literature biliary cyst-adenoma has a recurrence risk of 10% [11].
Intra-hepatic biliary cystadenoma is a rare tumor, with non-specific clinical presentation, undefined biology and difficult diagnosis. Combining clinical, biological and radiological data is often used to direct the diagnosis, but pathology confirmation is required. Complete surgical resection is preferred because of the high risk of malignant transformation and recurrence.
Authorship
Mosaab Ghannouchi, Amina Chaka, Seifeddine Ben Hammouda, Mohamed Ben khalifa and Asma Chaouech prepared the manuscript. Karim Nacef, Kamel Hleli and Moez Boudokhane: guided authors in writing the manuscript and proofread the final manuscript.
- Poggio P, Buonocore M. Cystic tumors of the liver: A practical approach. World J Gastroenterol. 2008; 14: 3616. PubMed: https://pubmed.ncbi.nlm.nih.gov/18595127/
- Lau S, Kim S, Lee S, Schaller R. Mucinous cystadenoma of the pancreas in a one-year-old child. Journal Of Pediatric Surgery. 2004; 39: 1574-1575. PubMed: https://pubmed.ncbi.nlm.nih.gov/15486909/
- Tran S, Berman L, Wadhwani N, Browne M. Hepatobiliary cystadenoma: a rare pediatric tumor. Pediatr Surg Int. 2013; 29: 841-845. PubMed: https://pubmed.ncbi.nlm.nih.gov/23483342/
- Mortelé K, Ros P. Cystic Focal Liver Lesions in the Adult: Differential CT and MR Imaging Features. Radiographics. 2001 ; 2: 895-910. PubMed: https://pubmed.ncbi.nlm.nih.gov/11452064/
- Tran S, Berman L, Wadhwani N, Browne M. Hepatobiliary cystadenoma: a rare pediatric tumor. Pediatr Surg Int. 2013; 29: 841-845. PubMed: https://pubmed.ncbi.nlm.nih.gov/23483342/
- Thomas K, Welch D, Trueblood A, Sulur P, Wise P, Gorden D. et al. Effective Treatment of Biliary Cystadenoma. Annals Of Surgery. 2005; 241: 769-775. PubMed: https://pubmed.ncbi.nlm.nih.gov/15849512/
- Kanamori H, Kawahara H, Oh S, Mine T, Osawa H, et al. A case of biliary cystadenocarcinoma with recurrent jaundice. Diagnostic evaluation of computed tomography. Cancer. 1985; 55: 2722-2724. PubMed: https://pubmed.ncbi.nlm.nih.gov/3995481/
- Joel J. Biliary Cystadenoma: A Case Report. J Clin Diagnostic Res. 2016; 10: ED19–ED20. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4800543/
- Schoonbroodt D, Horsmans Y, Gigot J, Rahier J, Geubel A. Bili0ary cystadenoma of the liver with elevated CA 19-9. Liver. 2008; 14: 320-322. PubMed: https://pubmed.ncbi.nlm.nih.gov/7877437/
- Quigley B, Reid M, Pehlivanoglu B, Squires M, Maithel S, et al. Hepatobiliary Mucinous Cystic Neoplasms With Ovarian Type Stroma (So-Called “Hepatobiliary Cystadenoma/Cystadenocarcinoma”). Am J Surg Pathol. 2018; 42: 95-102. PubMed: https://pubmed.ncbi.nlm.nih.gov/29016404/
- Boytchev I, Georgelin M, Bedossa P, Buffet C. Cystadénocarcinome biliaire intra-hépatique. Gastroentérologie clinique et biologique. 1999; 23: 981-983.
- Lewis WD, Jenkins RL, Rossi RL, Munson L, ReMine SG, et al. Surgical treatment of biliary cystadenoma: a report of 15 cases. Arch Surg. 1988; 123: 563-568. PubMed: https://pubmed.ncbi.nlm.nih.gov/3358682/