More Information
Submitted: November 20, 2023 | Approved: December 26, 2023 | Published: December 27, 2023
How to cite this article: Amitrano L, Guardascione MA, Saviano S, Martino A and Lombardi G. Bleeding from Varices: Still a Heavy Burden in Patients with Cirrhosis. Ann Clin Gastroenterol Hepatol. 2023; 7: 035-037.
DOI: 10.29328/journal.acgh.1001043
Copyright License: © 2023 Amitrano L, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Varices; Bleeding; Cirrhosis
Bleeding from Varices: Still a Heavy Burden in Patients with Cirrhosis
Amitrano L*, Guardascione MA, Saviano S, Martino A and Lombardi G
Gastroenterology Unit, AORN Antonio Cardarelli, Naples, Italy
*Address for Correspondence: Lucio Amitrano, Via Morghen 92 Naples, Gastroenterology Unit, AORN Antonio Cardarelli, Naples, Italy, Email: [email protected]
Introduction: Bleeding from varices is a severe complication in patients with cirrhosis. Despite its treatment has been well established in the last three decades the mortality can be still high. This study compares the epidemiological features and the bleeding-related outcomes of a group of patients published about ten years ago with a more recent group of 168 consecutive patients.
Methods: The diagnosis, the treatment, and the main outcomes (5-day failure, 5-day and 6-week rebleeding, 5-day and 6-week mortality) of variceal bleeding were evaluated according to the current guidelines.
Results: The number of patients with cirrhosis admitted for variceal bleeding every year has progressively decreased in the last ten years. The age sex and severity of liver disease, evaluated with Child Pugh and MELD scores, were comparable in the two series. In the more recent series, there were significantly fewer patients with HCV infection and more patients with alcohol-related cirrhosis. The main outcomes of bleeding were comparable too. Overall, at 6 weeks 36.4% of patients did not overcome the bleeding episode.
Conclusion: The decreasing incidence of bleeding from varices is likely attributable to antiviral treatment of HCV and HBV and the larger diffusion of beta-blockers in primary prophylaxis. Despite the larger application of the gold standard therapy, the mortality of variceal bleeding remains high in patients with cirrhosis.
The treatment of bleeding from esophagogastric varices in patients with liver cirrhosis has been well-established over the past decades. Despite the widespread use of the combination of vasoactive-antibiotics and endoscopic therapy the mortality at the acute episode is still relevant [1].
In 2012 our group published a paper on the outcomes of a large group of unselected patients bleeding from varices (group 1) [2].
Since then several epidemiological and therapeutic changes have occurred in the universe of chronic liver disease as the early identification and the evident increase of fatty liver disease and its consequences, the diffusion of antiviral therapy for HCV, the advisable larger use of beta-blockers in the primary prophylaxis of variceal bleeding.
We retrospectively studied a group of consecutive patients admitted for variceal bleeding from January 1st, 2019 to December 31, 2020, compared to the previous one to identify changes in the epidemiological and clinical features and main outcomes of bleeding (group 2).
Group 2 consisted of two hundred-twenty-four consecutive patients admitted to the Gastroenterology Unit of AORN A. Cardarelli in Naples Italy because of variceal bleeding, esophageal 201 (90%), gastric 16 (7%), duodenal 7 (3%). Twenty-one patients were not evaluated because they had no liver cirrhosis, 4 had a previous TIPS inserted, 31 had an episode of late rebleeding and were considered once. Overall 168 patients were considered. The standard treatment of bleeding in cirrhotic patients has been previously described (2) and it has not changed in the last ten years. The main outcomes of bleeding (5-day failure, 5-day, and 6-week rebleeding. 5-day and 6-week mortality) are reported according to Baveno [3-4].
Categorical variables were compared using the Chi-squared test and continuous variables the unpaired Student ‘s t-test.
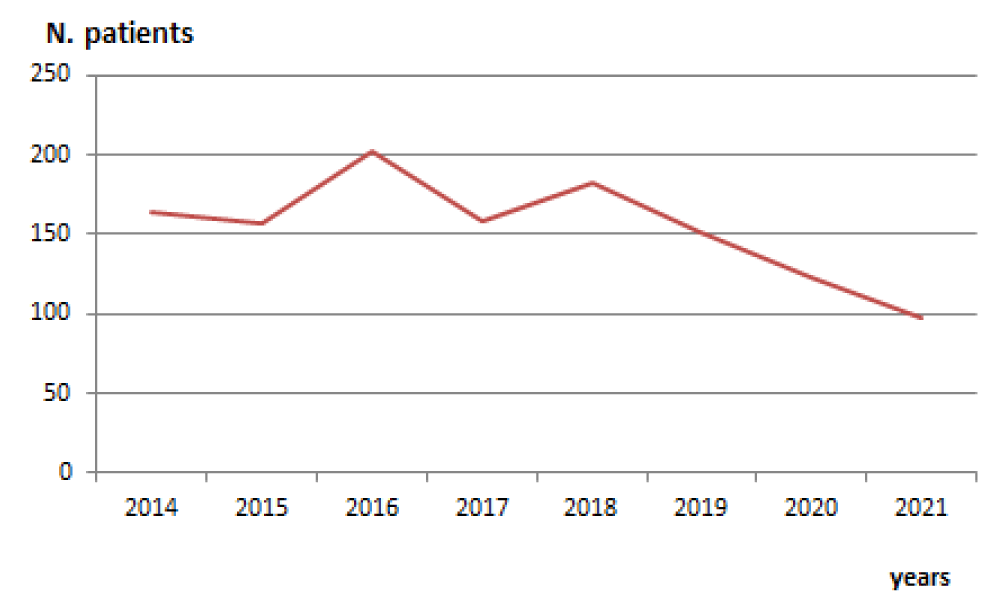
As shown in Figure 1, the number of patients admitted every year because of variceal bleeding has steadily decreased over the last few years.
Figure 1: Number of cirrhotic patients bleeding from varices yearly admitted to the Gastroenterology Unit of AORN A. Cardarelli Hospital in Naples.
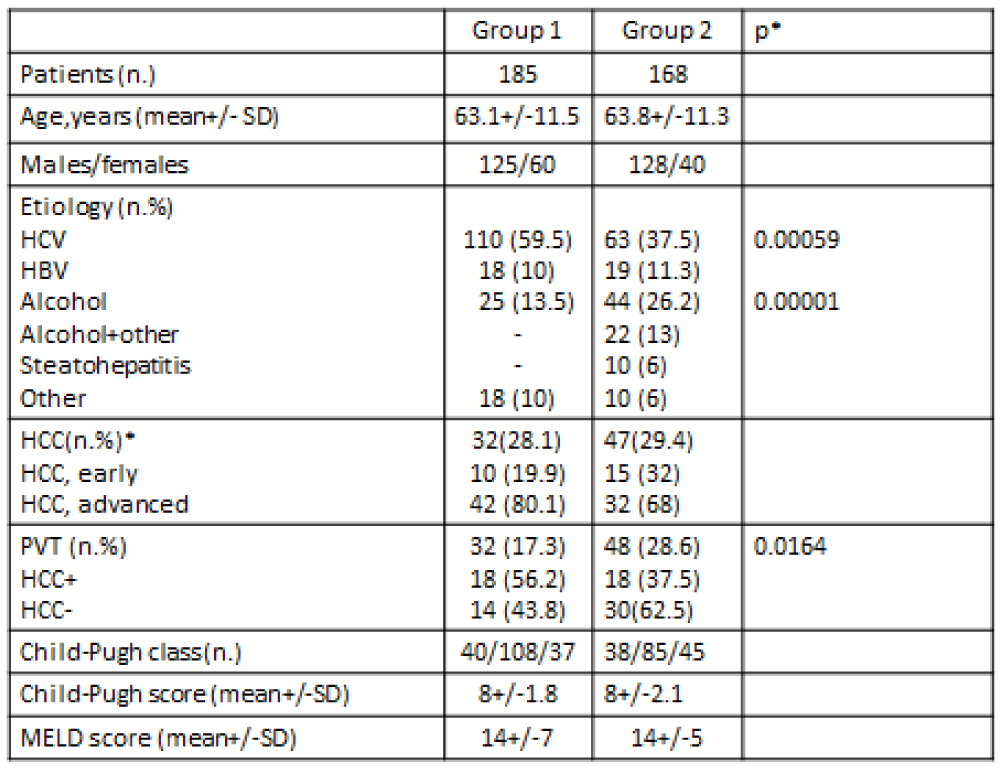
The main features of group 2 vs. group 1 are compared in Table 1. Age (63.1+/-11.5 vs. 63.8+/-11.3 yrs.), gender (M/F 125/60 vs. 128/40), number of patients with HCC (28.1% 29.4%), Child-Pugh (8+/-1.8 vs. 8+/-2.1) and MELD score (14+/-7 vs. 14+/-5) were not different. In group 2 there were significantly fewer patients with HCV (37.5% vs. 59.5%, p < 0.01) and significantly more patients with alcohol-related disease (39.2% vs. 13.5%, p < 0.01). The group of patients with cirrhosis due to steatohepatitis has been better defined and more included in the group of “other” etiology where rarer causes of liver disease are concerned.
Table 1: Epidemiological and clinical features of the two cohorts of cirrhotic patients bleeding from varices.
The prevalence of portal vein thrombosis was increased (28.6% vs. 17.3%, p < 0.05).
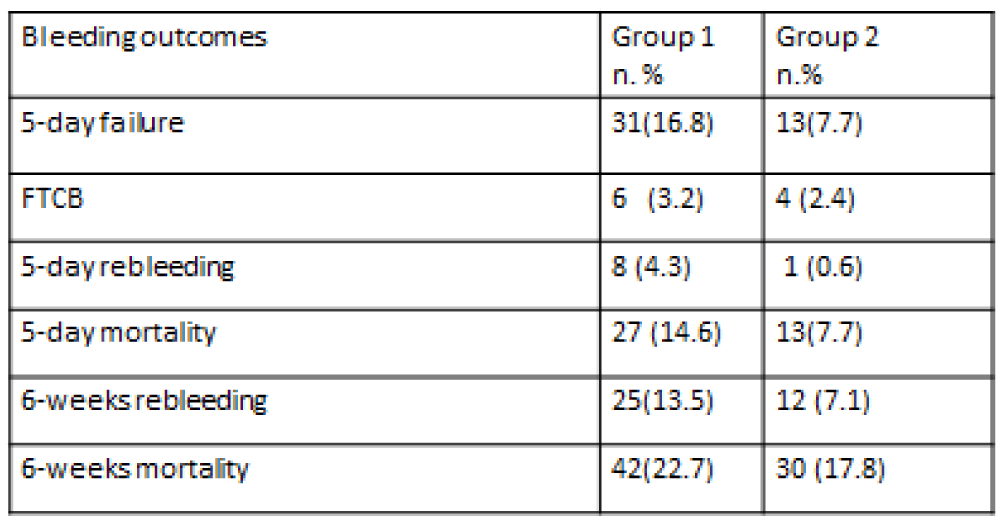
The main outcomes of the bleeding episode showed an overall further improvement (Table 2).
Table 2: The main outcomes after bleeding from varices in the two cohorts. FTCB= failure to control bleeding.
As for as mortality is concerned eight patients (4.5%) presented with gastrointestinal bleeding presumably from portal hypertension and a decompensated liver disease in very poor clinical conditions or hemodynamic instability to be judged not suitable for endoscopy and died early after admission, 7.7% of the patients died within 5 days and further 11.1% at six weeks. Moreover, 13% of the initial population worsened heavily after bleeding so that was not able to face the varices eradication program because of liver decompensation or advanced HCC.
Overall, 36.4% of the population died or was too ill at six weeks after the index bleeding.
We report a decreased number of patients admitted for variceal bleeding over the last years despite epidemiological data showing an overall increase in the prevalence of liver cirrhosis [5] paralleled by a decrease in the mortality in some geographical areas [6].
The changes in the etiology of liver disease with a stable prevalence of HBV but a clear decrease of HCV-related cirrhosis, likely secondary to antiviral treatment, may have contributed to these results.
Moreover, in the last decades, better identification of steatohepatitis-related cirrhosis has occurred together with an increase in its prevalence as occurred in our series. Lastly, the larger diffusion of beta-blockers in primary prophylaxis may have had a role in decreasing the number of patients presenting with bleeding.
The stage of hepatic insufficiency, expressed by Child-Pugh and MELD score, at hemorrhage, did not change, bleeding affecting mostly patients with moderate and severe disease. Of which about one-third were confirmed to have HCC. In addition, more patients were diagnosed to have PVT indicating not only a more advanced disease but also the fact that this complication is nowadays systematically searched.
The main outcomes of bleeding further ameliorated likely because of the larger expertise in the endoscopic treatment of bleeding and the clinical management of the medical complications of cirrhosis. Despite this if we consider the interval of 6 weeks in which bleeding had its effects on liver function 36.4% of patients did not overcome the bleeding episode.
The overall impact of variceal bleeding on the course of liver disease is still dramatically heavy particularly in advanced cases.
- de Franchis R, Bosch J, Garcia-Tsao G, Reiberger T, Ripoll C; Baveno VII Faculty. Baveno VII - Renewing consensus in portal hypertension. J Hepatol. 2022 Apr;76(4):959-974. doi: 10.1016/j.jhep.2021.12.022. Epub 2021 Dec 30. Erratum in: J Hepatol. 2022 Apr 14;: PMID: 35120736.
- Amitrano L, Guardascione MA, Manguso F, Bennato R, Bove A, DeNucci C, Lombardi G, Martino R, Menchise A, Orsini L, Picascia S, Riccio E. The effectiveness of current acute variceal bleed treatments in unselected cirrhotic patients: refining short-term prognosis and risk factors. Am J Gastroenterol. 2012 Dec;107(12):1872-8. doi: 10.1038/ajg.2012.313. Epub 2012 Sep 25. PMID: 23007003.
- de Franchis R . Developing consensus in portal hypertension. J Hepatol 1996 ; 25 : 390 – 4
- de Franchis R . Evolving consensus in portal hypertension. Report of the Baveno IV Consensus Workshop on definitions, methodology and therapeutic strategies in portal hypertension. J Hepatol 2005; 43 : 167 – 76
- Liu YB, Chen MK. Epidemiology of liver cirrhosis and associated complications: Current knowledge and future directions.W J Gastroenterol 2022; 28: 5910-30
- Cheemerla S, Balakrishnan B. Global Epidemiology of Chronic Liver Disease. Clin Liv Dis 2021:17: 365-70